Unlocking Orthostatic Hypertension’s Silent Stranglehold on Cardiorenal Harmony
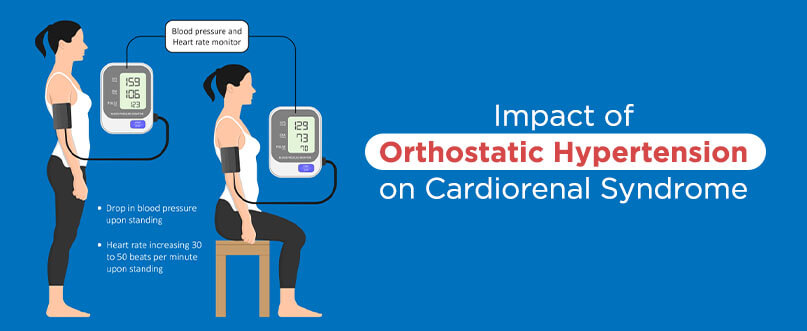
Orthostatic hypertension (OHT) is an increase in the blood pressure on assuming an upright position. It is a clinical problem increasingly observed in people who suffer from borderline hypertension, diabetes mellitus, autonomic neuropathies, and among the elderly. However, OHT remains understudied and under-recognised in clinical practices because of its atypical nature.
Cardiorenal syndrome (CRS) includes a range of disorders that involve both the heart and kidneys, where acute or chronic dysfunction in one of the organs may cause acute or chronic dysfunction in the other organ. It is a convergence of heart-kidney interactions across several interfaces.
The association of OHT with the progression of organ damage and increased incidence of chronic kidney disease (CKD) and coronary heart disease is gaining attention though not to a sufficient extent.
In a study conducted on healthy airmen, 4.2% had OHT. Another study conducted on subjects with type-2 diabetes in Japan found that the prevalence of OHT was significantly higher in diabetic patients than in control subjects; it was 12.8 vs 1.8%. The prevalence of OHT in a group of patients with long-standing type-1 diabetes was 15.2%
Things To Know About Orthostatic Hypertension And Cardiorenal Syndrome
High blood pressure, or hypertension, is when the bodily blood pressure is consistently higher than normal. There are two types of hypertension. For 95% suffering from hypertension, the cause is unknown, known as primary or essential hypertension. When it is possible to establish the reason, it is known as secondary hypertension.
Orthostatic hypertension has no standard definition yet, but an operational purpose is available based on previous studies.
Cardiorenal Syndrome is a group of different clinical conditions in which heart and kidney dysfunction overlap as per the Consensus Conference on Acute Dialysis Quality Initiative Group.
- Type 1 CRS is indicated by acute worsening of cardiac function leading to acute kidney injury (AKI).
- Type 2 2 CRS occurs against the backdrop of chronic heart disease.
- Type 3 CRS is closely related to AKI.
- Type 4 CRS refers to cardiovascular involvement in those suffering from chronic kidney disease.
- Type 5 CRS denotes cardiac and renal involvement in several diseases.
Orthostatic Hypertension Symptoms
Orthostatic hypertension rarely exhibits clinical symptoms. It is essential for clinicians, especially cardiologists and physicians in the emergency room, to diagnose this condition correctly.
Mild OHT may be present without any symptoms. Severe OHT patients show signs the same as hypertension.
Orthostatic hypertension symptoms may be absent in mild or moderate cases, but the symptoms may be the same as hypertension BP findings. Orthostatic venous pooling is common with orthostatic diastolic hypertension. It occurs in the legs while standing.
Diagnosis And Detection Of Orthostatic Hypertension
The absence of a consensus regarding the definition of OHT makes it challenging to have a universally accepted approach to its diagnosis.
No consensus is available in the diagnostic workup and management of orthostatic hypertension. For diagnosing OHT, the search should focus on identifying surgically correctable causes of hypertension or ruling out baroreflex failure based on the previous studies.
A simple clinical test is a screening tool for orthostatic hypertension. The test includes resting for 5 minutes in the supine position, followed by BP measurement for 3 minutes during active standing. The pulse rate also gets recorded.
The Head-up tilt table test finds applications in cases where the active standing test provides inconclusive results. The patients are tilted with the head-up to 60° to 70° while monitoring their blood pressure continuously for 20 minutes.
The head-up tilt is not a screening tool for clinical routine but is a confirmatory test applied in selected cases.
Impact of Orthostatic Hypertension on Heart and Kidney
Many clinical conditions may be associated with ortho hypertension. Some are hypertension, medullary vascular compression, type 2 diabetes, nephroptosis, and dysautonomia/autonomic dysfunction. OHT is related to neuropathy in diabetes mellitus and an increased incidence of silent central nervous system ischemia.
OHT impacts the kidneys and is connected to Chronic Kidney Diseases (CKD). Patients exhibiting an orthostatic rise in BP >7.8 mm Hg have higher urinary albumin to creatinine ratio. The presence of microalbuminuria is a risk factor for the onset of renal disease in diabetic individuals and indicates increased mortality rates. In non-diabetic patients, microalbuminuria can predict CVD and peripheral vascular disease in the future.
Inflated sympathetic stimulation and baroreflex hypersensitivity are considered the pathogenesis of OHT. These factors also contribute to the risk and outcomes of Cardio Vascular Diseases patients. OHT is linked to increased brain natriuretic peptide, leading to increased left-ventricular systolic load.
Treatment And Management
1. Non-Pharmacological Options
Patients with orthostatic hypertension should avoid sudden changes in posture. Gravitational pooling is a significant factor for most OHT patients with no underlying cause. Decreasing this pooling with the use of anti-gravity suits could minimise orthostatic fluctuation.
2. Pharmacological Options
The α-adrenergic activity is the predominant pathophysiological mechanism in patients with OHT with no associated secondary causes. In a study on elderly hypertensives, α-adrenergic blockade decreased the orthostatic response.
Patients with substantial OHT are recommended α-adrenergic blockers. Clonidine, a centrally acting α2-agonist, lowers norepinephrine levels in patients with baroreflex failure. It also reduces hypertensive episodes. Recent studies have shown that the new calcium channel blocker azelnidipine has a more significant effect on baroreflex sensitivity than older analogues like amlodipine.
OHT is also considered a strong predictor of CVD death in patients above 80 years.
Conclusion
Orthostatic hypertension is a condition of postural regulation of blood pressure. OHT has a significant prevalence, and most studies point towards a close link between OHT and target organ damage.
Though the treatment options are pretty limited due to a lack of studies based on intervention, patients once diagnosed should undergo counselling similar to patients with orthostatic hypotension.
You can get helpful information and tips for effectively managing your blood pressure by following this link BPinControl. BPinControl offers you comprehensive information on hypertension, expert advice, and practical lifestyle tips. They offer consultations with physicians and a nutritionist to provide the proper guidance and support.
Note of caution: This article is for information purposes only. Always consult your doctor before altering any diet plans, medications or in case of any other blood pressure-related troubles.

Comments (0)
No comments found.Add your comment